A common test, currently used to determine whether patients who have previously suffered one or more heart attacks should undergo bypass surgery, is actually inconclusive and should not be relied on solely for the decision, according to a new study published today in the The New England Journal of Medicine.
Julio A. Panza, MD, Chief of Cardiology at Westchester Medical Center Health Network (WMCHealth), led the study of Myocardial Viability testing, which found that a more comprehensive and personalized assessment of each patient's ischemic cardiomyopathy using a number of determinants should be undertaken in order to determine the indication for cardiac bypass surgery.
The population of patients with ischemic cardiomyopathy - the condition in which the heart muscle is significantly weakened as a result of previous heart attacks - is growing, primarily as a result of the advances in medicine that have led to improved survival after a heart attack. This study is the product of a more than 20-year-long investigative effort into the role of bypass surgery in patients with coronary artery disease and left ventricular dysfunction.
The study consisted of 601 patients suffering from ischemic cardiomyopathy and it focused on the ways in which doctors can identify patients who benefit most from the high-risk intervention of bypass surgery.
Because bypass surgery has a higher mortality in this high-risk population of patients, a key issue is the identification of patients more likely to benefit from this high-risk surgery, while sparing those who would not benefit from the same operation.
The study confirmed that bypass surgery is beneficial in the long run (median follow-up was 10 years); however, it was found that the results of myocardial viability testing should not be the sole determinant of whether or not patients should undergo bypass surgery. In conjunction with the findings from other studies by the same investigators, the findings suggest that patients with ischemic cardiomyopathy should be recommended to undergo bypass surgery based on the extent of their coronary disease rather than on the results of tests assessing myocardial viability.
"We hope the findings of this study will be utilized to better understand the complexity of the clinical problem in this high-risk population of patients and help define the patients' needs for cardiac bypass surgery," said Dr. Panza.
The study was an international, multi-center effort funded by the National Institutes of Health (NIH) as a part of a larger trial called STICH (Surgical Treatment of Ischemic Heart Failure), the main results of which appeared in The New England Journal of Medicine in 2016. The results of the myocardial viability study will appear in the August 22 edition of The New England Journal of Medicine.
Dr. Panza is Chief of Cardiology at WMCHealth and the WMCHealth Heart and Vascular Institute is a multi-specialty practice dedicated to providing comprehensive, high-quality cardiac and vascular services. It brings together many of the nation's best physicians in cardiology, cardiovascular surgery, cardiothoracic surgery and pediatric cardiovascular services, practicing in state-of-the-art facilities. Highly trained teams of specialists, nurses, physician assistants and allied health professionals work together to provide a seamless continuum of care across WMCHealth's 10 hospitals on eight campuses.
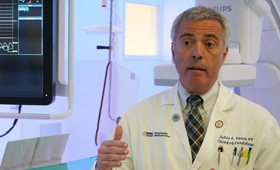
Julio A. Panza, MD, Chief of Cardiology at WMCHealth, is the lead author of the study published in The New England Journal of Medicine